We aim to provide you with the best quality care from our team of specialists, covering all the major sub-specialties of ophthalmology.
Our modern one-stop cataract service meets all the benchmarks of a ‘Gold Standard’ service, as set out by the Department of Health. You can find out more about cataract surgery by watching our video below.
You can find details of all our specialist services here, and you may find further information on specific conditions on our Patient Information Leaflets page.
Glaucoma is a condition that can gradually interfere with your vision, usually starting at the edges (peripheral vision).
You may not notice anything is wrong initially, and it is often picked up at a routine test at your opticians. More information can be found at Glaucoma UK - https://glaucoma.uk/
How do I arrange an appointment?
Your GP can arrange an appointment for you. It is important to have a regular appointment with your optician who should be able to detect the early signs of glaucoma at routine eye tests. Your optician can alert your GP of any signs.
What happens in a glaucoma clinic?
After your vision has been tested on the eye chart, you are often required to have a visual field test (a test of peripheral vision). This involves sitting in front of a screen and pressing a button each time you see a light. You will then see the doctor who will examine your eye and check your eye pressure.
Your eye pressure will be measured by applanation tonometry, where your eye is numbed with drops, and a lens very gently touches the front of your eye to take readings. You will need to have a special test called gonioscopy to judge the health of your drainage system inside your eye.
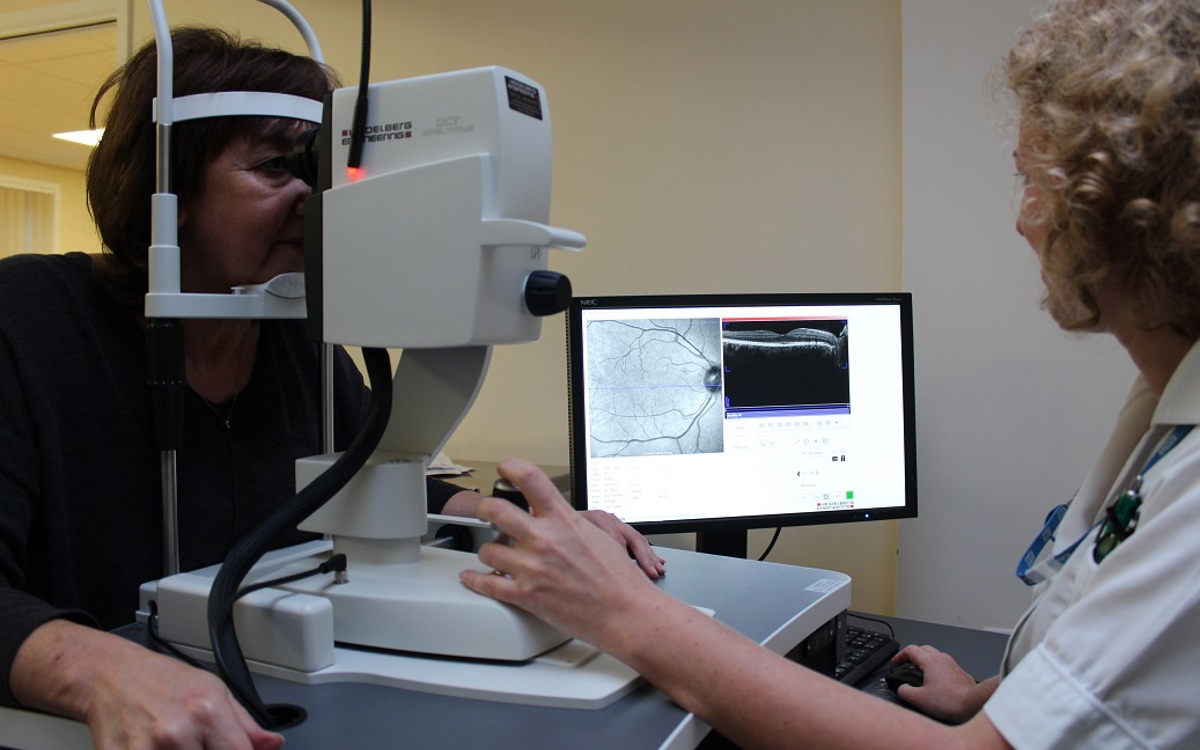
You may need a special image taking of your eye (similar to a photograph). The eye drops used often leave you with blurry vision for several hours afterwards, so you should not drive yourself home from the clinic.
If glaucoma is confirmed, you may be prescribed eye drops to control the eye pressure. This will be explained to you in the clinic. Patients with glaucoma often need to take eye drops every day, and to return for periodic check-ups.
Occasionally, in some patients the drops do not work well enough. Other options are available including laser treatment or surgery. These would be discussed with you if necessary.
Driving and glaucoma
Most patients who have glaucoma need to inform the DVLA about their diagnosis.
The DVLA often arrange special tests (visual field tests), which can be done at a local opticians. Please see the DVLA website for the latest guidance; https://www.gov.uk/government/organisations/driver-and-vehicle-licensing-agency
Cataract means a cloudy lens inside the eye. These often cause blurred vision, and become progressively worse over time. They can occur at any age, but are more common as you get older. Cataracts can be removed with surgery to improve vision in the majority of cases.
How do I arrange an appointment?
Your optician or GP can arrange an appointment. If you are concerned that your vision is getting gradually worse, it is sensible to see your optician promptly, so that a referral can be made for you.
How will my cataract be treated?
New patients are seen at the Cataract Clinic on Windsor Suite, where you will first have some vision tests, and measurements by our Specialist Nurses. You will then see the doctor who will examine your eyes and discuss your condition in more detail. Drops will be used to dilate your pupils and these will mean your vision is blurred for a few hours afterwards.
If cataracts are confirmed, and you choose to have surgery you will usually then be able to choose a date for your surgery that is convenient for you. This is normally available within three months.
We offer modern cataract surgery with the latest small incision techniques. This is performed under local anaesthesia in 99% of patients, as a day case (i.e you do not need to stay in hospital). There is usually no need for an injection, with eye drops alone used to numb the eye. Some people have medical conditions that mean it is safer to be given a general anaesthetic (be asleep for the surgery). This is possible, and would be discussed with you by the doctor.
After the surgery you are given eye drops to use for a few weeks, and usually return for a check up within a few weeks.
For more information please see our Cataract leaflet, available via the leaflet link below - please select the Ophthalmology drop down.
Please see below for a video explaining more. Please be aware this video contains graphic images of eye surgery.
Please watch our video to find out more about cataract surgery.
Please be aware this video contains images of surgery being carried out.
There are many different conditions that can affect the front part of the eye. The conjunctiva (skin covering the eye), the cornea (clear window at the front of the eye) and the sclera (the white coat of the eye) can all be damaged by disease. Some of these conditions cause pain, some can reduce the vision, and all of these are seen in the Cornea Clinic.
What happens in the cornea clinic?
Your vision will be tested by our specialist nurses. You may also need special measurements to be taken of your eye to measure the shape of the front of your eye (corneal tomography) – this is similar to having a photograph taken.
Depending on your condition, some patients are seen by the doctor, some by the contact lens practitioner, others by the specialist nurses, or a combination of these. You will sometimes need to have eye drops that can leave your vision blurred for a few hours afterwards, so you should not drive yourself home from the clinic.
You may be prescribed eye drops or other medication for your condition. These will be explained to you by the doctor or nurse.
Cornea Transplantation
If the clear window (cornea) of your eye becomes cloudy, your vision will become blurred. Sometimes surgery can be necessary to restore vision. A corneal transplant (also called a corneal graft or keratoplasty), is an operation to replace this cloudy cornea with a clear one. Various types of corneal transplant are available at James Paget University Hospital.
Endothelial corneal transplantation
We are proud to have been the first centre in Norfolk to offer the latest modern technique of lamellar endothelial transplant – this is a new ‘small incision’ technique for some types of corneal disease.
The retina is the layer of nerve cells at the back of the eye. Common conditions affecting the retina include Age-related Macula Degeneration (AMD), diabetes, and retinal detachment.
We provide a fully comprehensive retinal service including micro-incisional vitrectomy surgery and Lucentis therapy for age-related macular degeneration (AMD).
Our retinal imaging equipment is state-of-the-art, allowing detailed assessment of retinal conditions and the use of new 'virtual clinics' for monitoring.
Retinal laser is delivered with a PASCAL laser system, which reduces any discomfort dramatically, and also speeds up and improves the accuracy of retinal laser treatments.
We have recently started using implants of a novel slow-release steroid drug called Ozurdex for retinal vein occlusions.
Wet Age Related Macular Degeneration (AMD)
Untreated this is the commonest cause of blindness in the UK amongst people over the age of 55. Early treatment is now extremely effective. If you notice straight lines looking distorted or develop blurred vision then see your optician who can arrange “fast track” referral through to our AMD service within one week for urgent treatment if needed.
Eyelid problems are common. These can be simple lumps or cysts, eyelid drooping or abnormal position, watery eyes, and various skin cancers.
In the oculoplastics clinic, our team provide a broad range of oculoplastics procedures:
Correcting common eye lid problems such as
- entropion (eye lid rolling in)
- ectropion (eye lid rolling out)
- ptosis (droopy top lids)
- Blepharoplasty surgery for excess upper lid skin
- One-stop eye lid cyst clinic
- Periocular cancer service with a rapid biopsy service and excision with reconstruction where necessary. Some complex cases involve a multi-disciplinary team linked via a tele-link with JPUH and NNUH where experts in dermatology, plastics, oculoplastics, radiotherapy, radiology and histopathology decide optimum treatment.
- The lacrimal service offers a range of treatments for watery eyes, ranging from eye drops, syringing and minor procedures to lacrimal bypass procedures (DCR) which can be performed endoscopically (with no skin incisions) or externally.
- Treatment and surgery for socket related problems related to removal of the eye.
- Specialist thyroid clinic, offering the latest treatments
A child can be referred to the Eye Clinic by their GP, optician, school nurse, or from a screening clinic. Our paediatric eye clinics are sessions dedicated to children, run by specialist medical and nursing staff, orthoptists and optometrists.
What to expect
Children:
Your child will initially have their vision tested by one of our team of orthoptists. Their eye movements and stereo (3D) vision may also be tested at the same time. Your child may then be seen by the medical team, for an assessment of their eyes.
This will involve looking into the eyes with some bright lights, and they may then need some eye drops. Some eye drops take up to 30 minutes to work, after which a further examination will be required.
A test for glasses prescription will often be done - either by the doctor or our optometrist. The whole process can take over an hour (but the clinic does have a play area!) after which you will have time to discuss the nature of the problem and its treatment with the doctor.
If your child is prescribed glasses, it is usually best for these to be worn full-time.
'Patching' (or 'occlusion') treatment is sometimes necessary to encourage the improvement of a 'lazy' (or "amblyopic") eye. The patch is worn over the good eye for periods of the day to allow the weaker eye to catch up. Your doctor and orthoptist will explain this to you if this is necessary.
Squint (or "strabismus") means mis-alignment of the eyes, such that the eyes are not straight. This occurs in a range of conditions in both children and adults. Sometimes glasses with prisms are helpful, and sometimes an operation can be done to correct a squint.
Adults:
Adults with squint, or mis-aligned eyes will first have their vision tested on a reading chart. You will then have your eye movements and alignment measured by one of our team of orthoptists. This involves, for example, plotting your eye movements on a chart by asking you to look at a grid in different direction of gaze.
You will then see the doctor, who will make a further examination of your eyes with a microscope and some further bright lights. You will usually need eye drops to dilate your pupils - these make your vision blurred for several hours afterwards, so it is important not to drive yourself to the clinic. After all the tests have been done, you will have time to discuss any treatment with the doctor.
The James Paget University Hospital is a teaching hospital and is proud of its strong links with the University of East Anglia (UEA).
A large number of students and trainees gain experience at the James Paget each year, and the Eye Department is a leader in this field.
Virtual-reality ophthalmic surgical simulator
Through a £100,000 investment the Eye Department now has a Virtual Reality Surgical Simulator (EyeSi) for cataract surgery - the latest technology enabling microsurgical training to take place in a virtual reality simulator, so trainees develop their skills in a safe environment. The JPUH was one of the first sites in the UK with a simulator, and we remain a regional leader in simulation training.
Post graduate Training
All our consultants are trainers of junior doctors at all levels. Attached to the department are Ophthalmologists, GPs, optometrists and orthoptists in training.
Through such training we are able to teach the next generation of eye care professionals, and also remain up to date with the latest developments through continued professional development of training team.
Regional training
Some of our trainee doctors are part of the regional East Anglia training rotation.
Article 14 – We are keen to support the development and training of our medical staff, to meet their training needs through flexible timetabling, and support their progress with regular appraisal and guidance.
Mr Tom Butler, Consultant Ophthalmologist, is a Surgical Skills Trainer at the Royal College of Ophthalmologists, London. He has set up and runs the Wet Lab and Surgical Simulator Facility in the postgraduate Education Centre at James Paget University Hospital. This regional resource is available for all regional trainees. To find out more or book a place for training, call 01493 452298.
Undergraduate Training
The department provides teaching and clinical experience for undergraduate medical students at UEA, during their 4th year of Medical School. The teaching is delivered by all trainers in the department several times a year. In addition our consultants regularly visit UEA to deliver clinical seminars.
Dr Radomir Babovic is Module 7 UEA Lead for Ophthalmology at James Paget University Hospital.
We are constantly increasing our research capacity, and the Eye Department at JPUH is now part of a number of on-going multi-centre national trials:
- Professor Ben Burton is developing retinal research in the eye department and is currently principle investigator on four industry-sponsored trials.
- Mr Avinash Prabhu is undertaking several studies in glaucoma research
- Mr Craig Goldsmith is involved in a trial of a new treatment for multiple sclerosis.
This activity generates funding for future research and allows us to purchase specialist equipment for the eye department. In addition our patients gain early access to new sight improving treatments, eg Lucentis for diabetic retinopathy, otherwise unavailable on the NHS.
Each of the consultant team have published prolifically, and regularly undertake trials, studies and papers in order to ensure that their knowledge and skills remain up to date.
In a challenging financial environment, there is always equipment that we are not able to fund through the NHS. In the past we have received very generous financial support from many patients and relatives, and as such we have established a charitable endowment fund to help us fund new equipment, and improve our services to you.
If you would like to make a donation to help support our services, we would be very grateful for any help you can give. Please send a cheque made payable to James Paget University Hospital NHS Foundation Trust, and write ‘Ophthalmic Endowment Fund’ on the reverse of the cheque. You can call 01493 452762 for further help.
Examples of purchases made with the help of such generous support include:
- Eye testing equipment for children – modern equipment for accurate measurement of vision in children.
- Digital corneal photography equipment – to allow high resolution images of the front of the eye to be documented.
- Glaucoma assessment software – to improve the management of patients with glaucoma.
- The latest software for accurate cataract lens measurement – to optimise our visual outcomes
- Virtual reality cataract surgery simulator – safely and effectively training surgeons and improving patient outcomes
- Oculoplastic surgery equipment.
- Ultrasound equipment – to allow the detailed assessment of internal structures in the eye.
